Overweight and obesity in Norway
Updated
|Approximately 1 in 4 middle-aged men and 1 in 5 women have obesity with a body mass index of 30 kg / m2 or higher in Norway. Among children, the proportion with overweight and obesity appears to have stabilised.
Main Points
- Overweight is a body mass index (BMI) between 25 and 30 kg / m2. Obesity is a BMI of 30 kg / m2 or above. Obesity is primarily associated with an increased health risk.
- In total, between 15 and 20 per cent of children are overweight or obese (about 1 in 6 children). There are signs that the trend has levelled out.
- In total, 1 in 4 young people (about 25 per cent) are overweight or obese. There are indications that the proportion is increasing.
- About 1 in 4 men and 1 in 5 women aged between 40-45 years are obese. The proportion has increased in the last 40-50 years. The proportion with overweight comes in addition to the proportion with obesity.
- The combined proportion with overweight and obesity varies by region and education level.
- A high BMI contributes to approximately 2400 annual deaths in Norway and probably many cases of cardiovascular disease, diabetes and other chronic diseases.
About overweight and obesity
There are several measurements for overweight and obesity:
Body mass index (BMI) is the most commonly used measurement for weight ratios in the population. BMI is calculated by dividing body weight by height squared, i.e. kg / (m x m). For adults, these values apply:
- BMI of 18.5-24.9 kg / m2 is defined as normal weight.
- BMI of 25.0-29.9 kg / m2 is defined as overweight
- BMI of 30 kg / m2 and higher is defined as obesity.
See the example in the fact box further down.
BMI works well as a measure of overweight and obesity in a population, but when used for individuals it can be misleading. For example, people with a lot of muscle tissue and those who have shrunk in height could be defined as obese even though they have a normal amount of body fat.
Waist circumference is used to determine whether a person has abdominal obesity.
Data sources
Data on overweight and obesity in Norway are collected from different studies, including the Child Growth Study (8-9 year olds), Health Studies in Nord-Trøndelag (adolescents and adults), Tromsø Health Studies (adolescents and adults), National Service Centre (young adults) and the SAMINOR health study.
In the Child Growth Study and the Health Studies in North Trøndelag and Tromsø, health professionals recorded the weight and height measurements. Such data are more reliable because self-reported data may include inaccurate weight and height measurements. However, self-reported data, for example from the National Service Centre, may be a good source for studying trends over time.
Below is a description of the status and trends of overweight and obesity among children, adolescents and adults in Norway:
Overweight and obesity in children
Results from health studies show that:
- In total, between 15 and 20 per cent of children are overweight or obese, equivalent to about 1 in 6 (Dvergsnes, 2009; Kolle, 2009; NIPH, 2017a; Juliusson, 2007).
- In third grade, 14 per cent of girls and 11 per cent of boys are overweight, while 3 per cent of girls and 2 per cent of boys are obese (NIPH, 2017a).
- In third grade, 6 per cent of boys and 8 per cent of girls have abdominal obesity (NIPH, 2016).
In Norway, third graders are 8-9 years old.
Trends over time for children
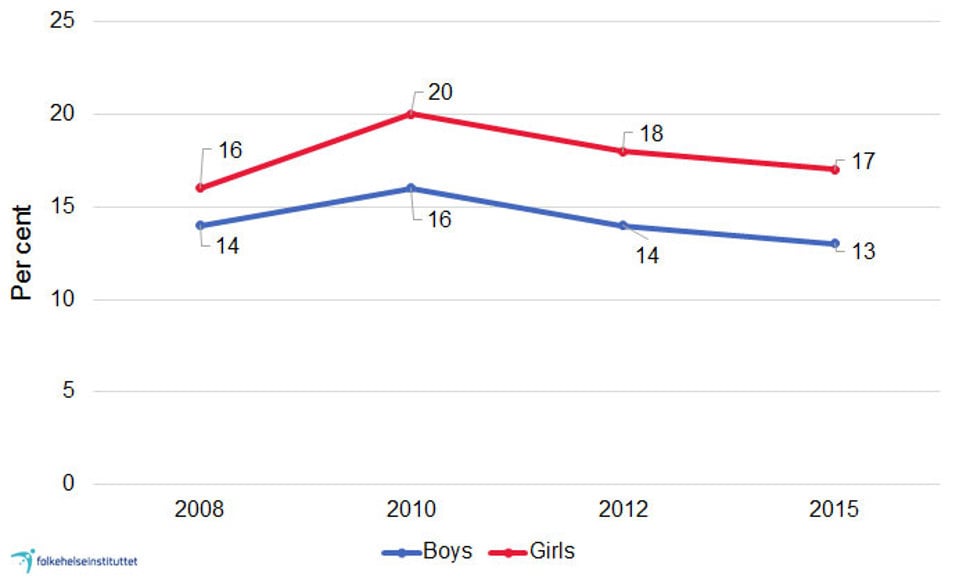
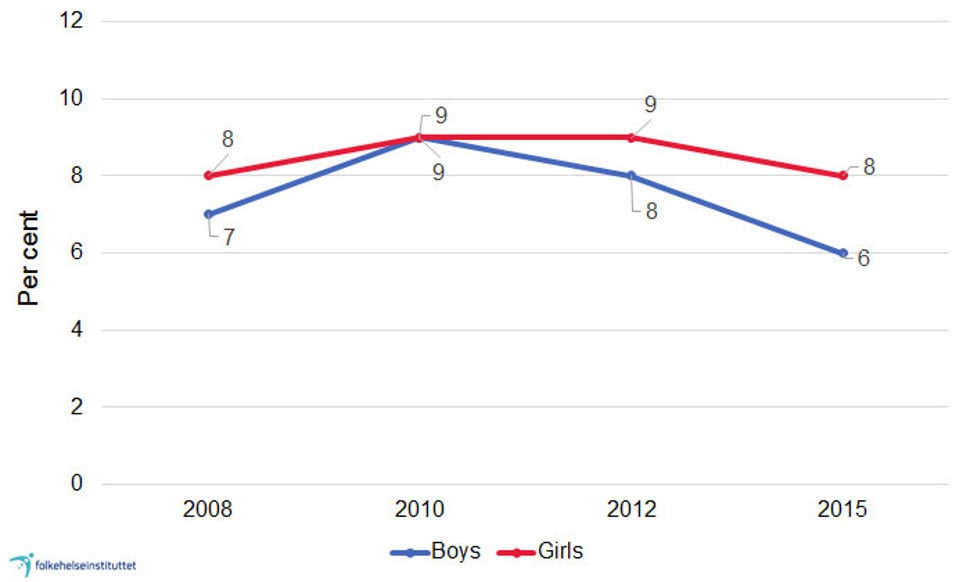
The percentage of overweight children increased from the start of the 2000s (Juliusson, 2007). However, in the last decade, it appears that the percentage of schoolchildren with overweight and obesity has not changed much, see Figure 1a and b, which shows figures from the Child Growth Study at the Norwegian Institute of Public Health.
Some studies indicate that, over a longer period, the average waist circumference has increased more than the average body mass index (BMI) (McCarthy, 2005), also in Norway (Kolle, 2009). However, according to the Child Growth Study in Norway, there were small changes from 2008 to 2015, see Figure 1b.
Overweight and obesity in adolescents
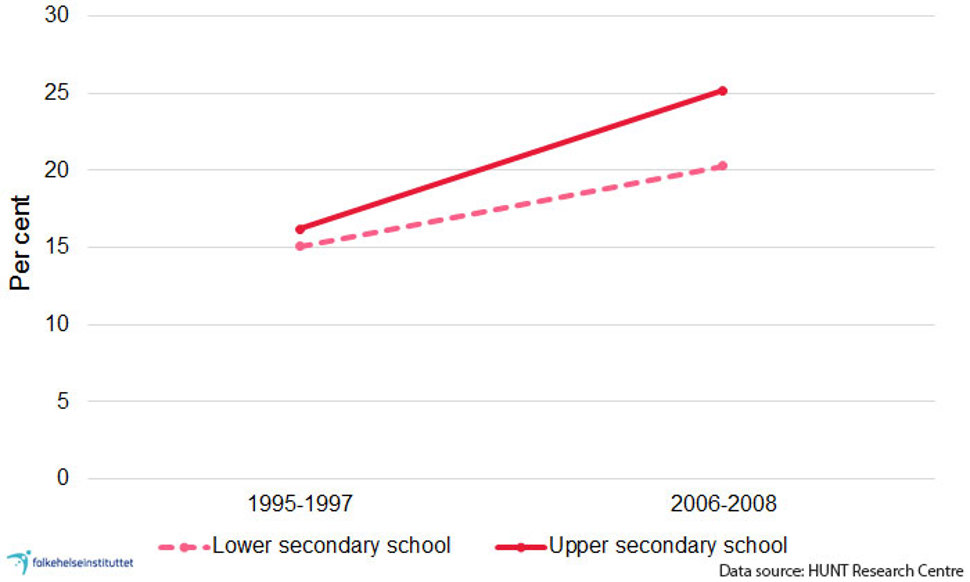
Results from the health study in Nord-Trøndelag (Young-HUNT 3) in 2006-2008 show that collectively speaking, about one in four adolescents are overweight or obese (HUNT Research Centre, 2011):
- 25 per cent of boys and 20 per cent of girls in lower secondary school are overweight or obese.
- 27 per cent of boys and 25 per cent of girls in upper secondary school are overweight or obese.
Contrary to the results from third graders in the Child Growth Study, where more girls than boys had overweight or obesity, the proportion of overweight or obesity is greatest among boys in both lower and upper secondary school.
Trends over time - adolescents and young adults
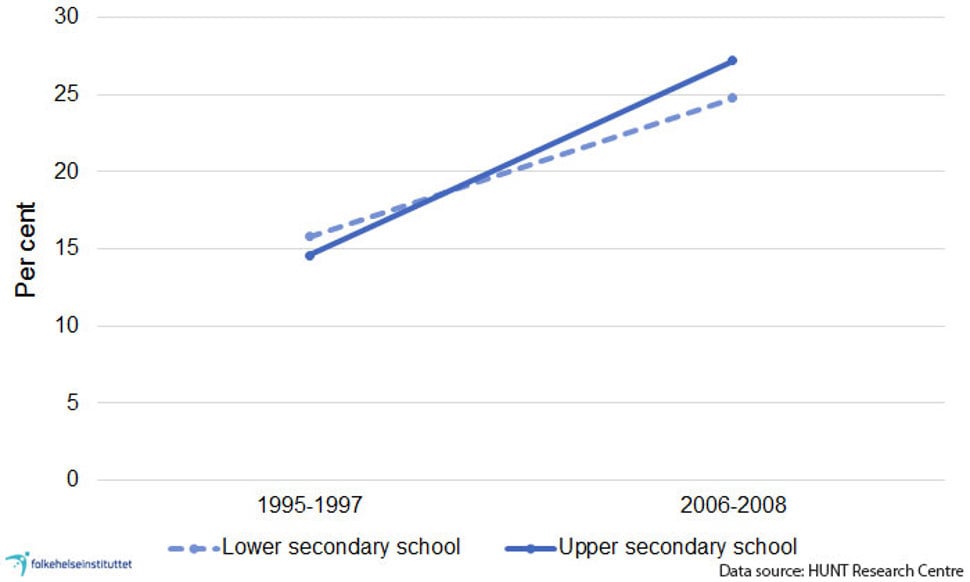
The proportion of overweight adolescents has increased in the last 40 years and continues to rise. This is a disturbing trend:
- 1995/1997 - 2006/2008: The average weight and the proportion of overweight or obese young people increased in Nord-Trøndelag until 2006-2008, see Figure 2a and b (HUNT Research Centre, 2011).
- 2012/2013: Tromsø study "Fit futures 2" shows that 21 per cent of young women and 28 per cent of young men aged 18-20 years are overweight or obese (Evensen, 2017).
Both in lower and upper secondary school there is a higher proportion of boys than girls who are obese. For boys this is 6 per cent in lower secondary school and 8 per cent in upper secondary school. For girls this is 4 per cent in lower secondary school and 5 per cent in upper secondary school (HUNT Research Centre, 2011).
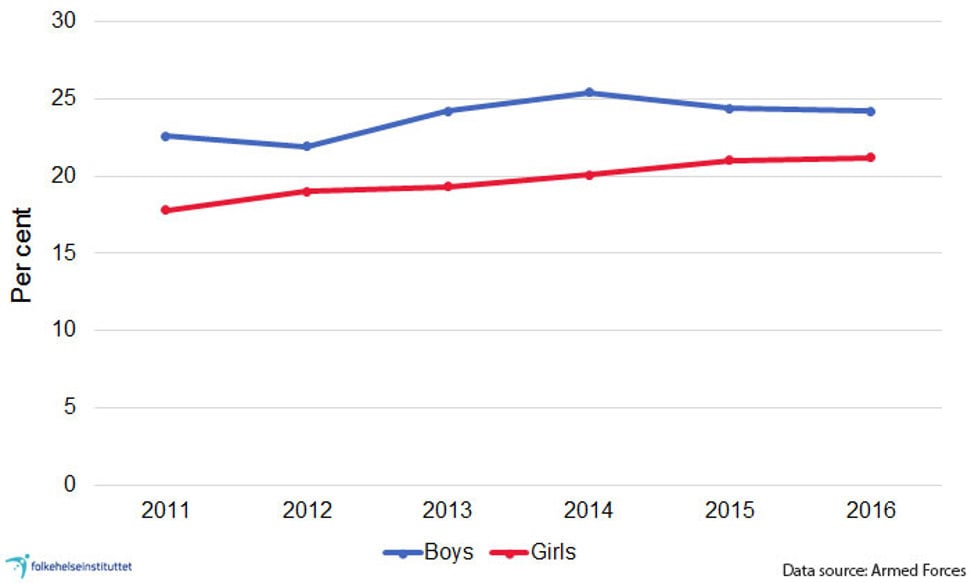
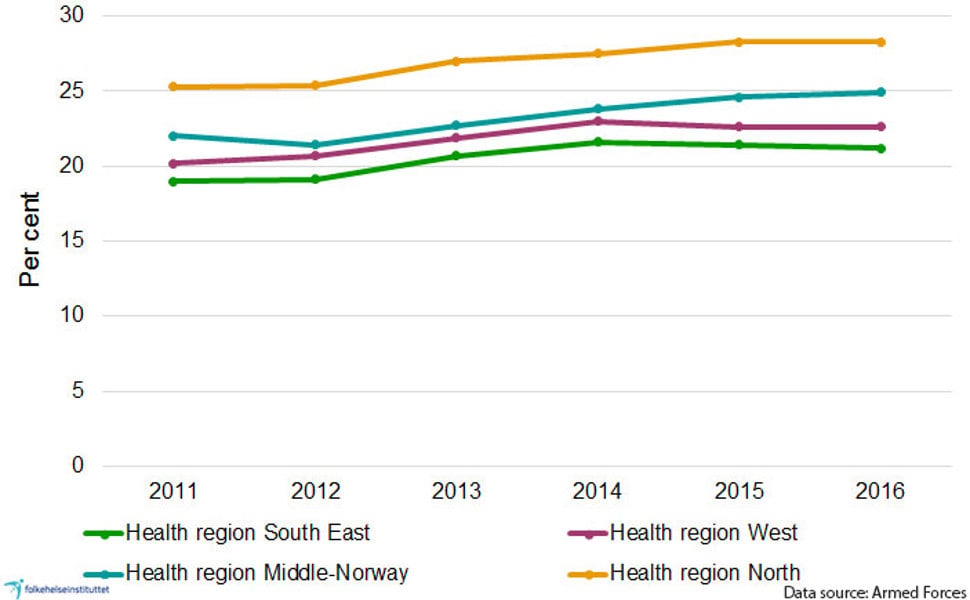
Session data from the Armed Forces indicate that the total proportion with overweight and obesity has increased slightly since 2008, see figure 3. The proportion may have stabilised in recent years. In terms of gender differences, session data also show that a higher proportion of boys than girls are obese (NIPH, 2017b). The figures are self-reported and should therefore be interpreted with caution.
Overweight and obesity in adults
The Tromsø study and the health study in Nord-Trøndelag indicate that most adults are either overweight or obese, and the minority have normal weight. We do not have national figures and the figures from the various studies are based on slightly different age groups, but these two studies from the period 2006-2008 (Jacobsen, 2015; Midthjell, 2013) and 2016 (unpublished figures from Jacobsen) show that:
- about 25 per cent of men and 40 per cent of women have normal weight
- the majority of men and women have overweight or obesity, the proportion is greatest among men.
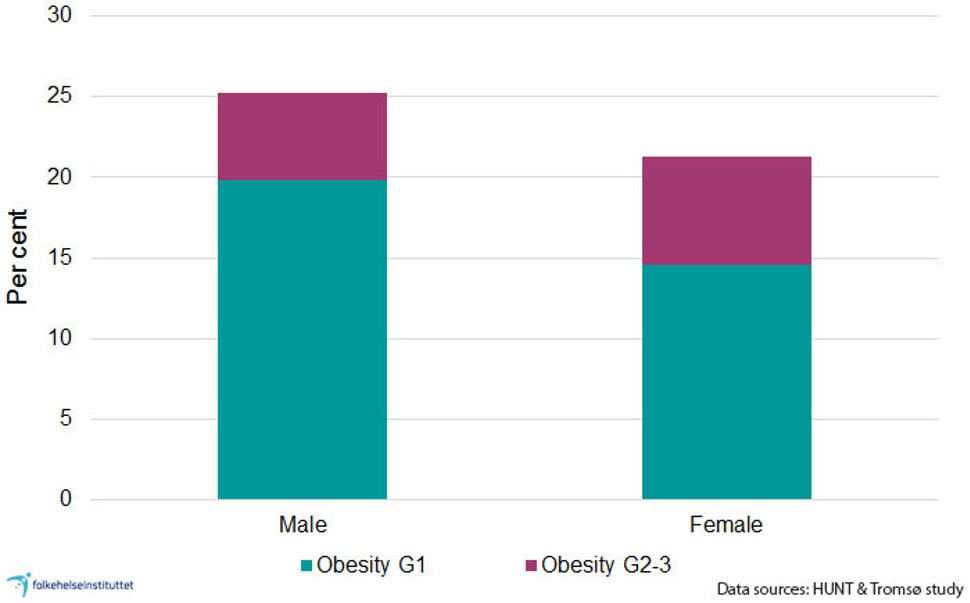
- about 25 per cent of men and 21 per cent of women aged 40-45 are obese, see Figure 4.
- in total, there is a greater proportion of men than women with obesity, but the percentage of grade 2 or grade 3 obesity (BMI ≥ 35 and 40 kg / m2) is higher among women than among men (6.7 per cent among females and 5.4 per cent among men), see figure 4.
If we extrapolate the results to the entire population in the 40-45 age group, it means that approximately 26,000 people have BMI ≥ 35 kg / m2 (grade 2 or grade 3 obesity). For a person who is 170 cm high, a weight of 101 kg gives a BMI of 35 kg / m2.
Waist circumference and the proportion with abdominal obesity are also increasing (Midthjell, 2013; Jacobsen, 2016). There are indications that the proportion with abdominal obesity is increasing more than can be explained by the increase in BMI itself (Jacobsen, 2016).
Data from the HUNT study suggest that among adults with BMI ≥ 35 kg / m2, nearly half of them (40-50 per cent) are morbidly obese, i.e. they have either health complications or BMI ≥ 40 kg / m2, (communication, Kristian Midthjell). See fact box below.
BMI = body mass index, which is an expression of weight relative to body surface area (height x height; m2). BMI is measured as kg/ m2.
Overweight:
- BMI 25.0–29.9 kg/ m2. A person who is 170 cm high and weighs 73 kg has passed the limit for overweight at 25 kg/ m2.
Obesity:
- BMI ≥ 30 kg/ m2
Obesity is divided into three subgroups:
- Obesity grade 1: BMI 30-34 kg / m2. Means in practice that weight is over 87 kg for a person who is 170 cm tall.
- Obesity grade 2: BMI 35-39 kg / m2. Means in practice that weight is over 101 kg for a person who is 170 cm high.
- Obesity Grade 3: BMI ≥ 40 kg / m2. Means in practice that weight is over 116 kg for a person who is 170 cm tall.
The term "morbidly obese" is used if BMI ≥ 40 kg / m2 or BMI ≥ 35 combined with health complications (sequelae).
Trends over time among adults
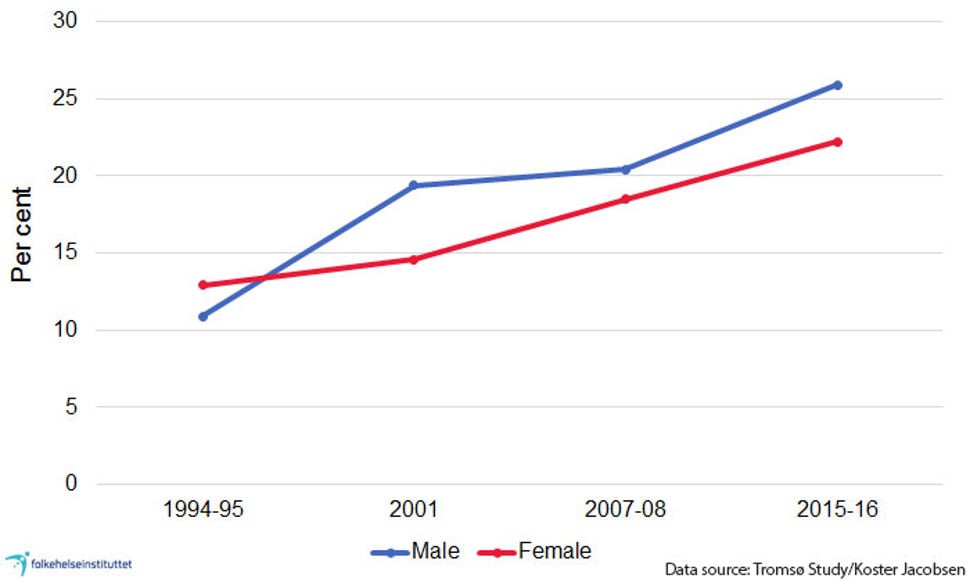
The proportion of adults with overweight or obesity has increased in the last 40-50 years.
Men:
- At the end of the 1960s, only approx. five per cent of Norwegian middle-aged men were obese.
- From around 1970, the average weight increased continuously until the turn of the millennium. The increase was particularly high at the end of the 1990s (Meyer, 2005).
Women:
- Among women, the percentage of obesity declined from 13 to 7 per cent in the period from the 1960s to the late 1970s.
- From around 1980, the average weight increased in the same way as for men (Meyer & Tverdal, 2005).
- Figure 5 shows how the prevalence of obesity has increased steadily in men and women in Tromsø over the past 20 years.
Differences between groups in the population
Geographical differences
The prevalence of overweight and obesity is lower in urban areas than in rural areas (Statistics Norway, 2016).
City and country. The proportion of overweight children is 50 per cent higher in rural areas than in cities. The percentage with abdominal obesity follows the same pattern (Biehl, 2013).
Geographical differences. The prevalence of overweight and obesity among children is the highest in Health Region North and lowest in Health Region South East, according to measurements from 2012 (NIPH, 2014).
Among 17-year-olds, the proportion with overweight and obesity is highest in Health Region North and the lowest in Health Region South East, see Figure 6 (NIPH, 2017b).
Figures from Oslo in 2000-2001 show that the adult population was heavier in eastern than in western suburbs, especially for women (Oslo Health Study in Oslo 2000-2001).
The Sami population
Data from the Sami population were collected from the SAMINOR 1 study in 2003-2004 and SAMINOR 2 in 2012-2014. Both health studies took place in an area with Sami and non-Sami populations.
A comparison between the studies in 2003/2004 and 2012/2014 shows that the proportion with obesity has increased both among Sami and non-Sami men, while the proportion has stabilised or decreased for women (unpublished data, Bent-Martin Eliassen).
Abdominal obesity has increased among both Sami and non-Sami men and women. Figures from 2003-2004 show that:
- a higher proportion of Sami than non-Sami men had BMI ≥30 while there was a lower proportion with abdominal obesity (waist circumference ≥102 cm)
- among Sami women, there was a higher proportion with both obesity measured with BMI and with abdominal obesity than in non-Sami women (waist circumference: ≥ 88 cm) (Nystad, 2010).
Data from 2012-14 indicate the same ethnic differences as ten years earlier.
Immigrant population
The prevalence of obesity varies among different groups of immigrants. The prevalence is high among immigrants from Pakistan and Turkey but low among immigrants from Vietnam. Women from Sri Lanka and Pakistan have most abdominal obesity and the highest prevalence of diabetes (NIPH, 2008).
Variation by education and family situation
The prevalence of overweight and obesity varies with education and family situation.
Adults: Among 40-year-olds, the percentage with obesity is lower among those with higher education than among those with lower education (Meyer, 2005). Figures among adults aged 25-79 years from the Living Conditions Survey in 2015 show the same (NIPH, 2017c).
Children and adolescents: There are also socioeconomic differences in overweight and obesity among children. The proportion of overweight is 30 per cent higher among children of mothers with lower education than among children of mothers with higher education. The percentage with abdominal obesity follows the same pattern (Biehl, 2013).
In the Child Growth Study 2010, the proportion with overweight and obesity was over 50 per cent higher among children with divorced parents compared to children with married parents (Biehl, 2014).
Among 15-year-olds, we also see the same differences between children with lower and higher education (UngKan study) (Norwegian Directorate of Health, 2012).
International differences
The weight increase that we have seen among children and adults in Norway is part of an international trend in which the proportion of overweight or obesity is increasing in many countries.
However, it appears that the prevalence of obesity among subjects is lower in Norway than in many other countries (OECD, 2012). Different methods have been used and there are different qualities in the studies used as the basis for the comparisons. It is therefore difficult to place Norway in the international rankings.
The USA was one of the countries where we first saw the trend of an increasing proportion with overweight and obesity. Among American children, it seems the proportion with overweight and obesity is no longer increasing, while it continues to increase among teenagers (Ogden, 2016). The proportion is higher than in Norway.
North-south gradient among children in Europe
In countries in southern parts of Europe, there is a much larger percentage of children with overweight and obesity than in Norway and other Nordic countries, see table 1 where figures from the Child Growth Study at the Norwegian Institute of Public Health are part of the data collection of the WHO European Childhood Obesity Surveillance Initiative.
|
Country |
Age group |
Proportion with overweight and obesity1 (%) |
Proportion with overweight and obesity1 (%) |
|
|
7-year-olds |
Boys |
Girls |
|
Sweden |
|
14.6 |
17.8 |
|
Latvia |
|
15.3 |
15.1 |
|
Lithuania |
|
16.1 |
16.2 |
|
Ireland |
|
21.1 |
22.8 |
|
Belgium |
|
15.2 |
19.4 |
|
Czech Republic |
|
15.8 |
14.7 |
|
Slovenia |
|
24.2 |
22.0 |
|
Bulgaria |
|
20.1 |
24.2 |
|
Portugal |
|
26.8 |
28.5 |
|
|
8-year-olds |
|
|
|
Norway |
|
13.5 |
17.4 |
|
Sweden |
|
17.4 |
17.9 |
|
Belgium |
|
13.9 |
17.4 |
|
Slovenia |
|
25.2 |
25.6 |
|
Italy |
|
37.2 |
34.7 |
Health risks associated with obesity
Over time, obesity gives an increased risk of developing a number of diseases and ailments (WHO, 2000; Norwegian Directorate of Health, 2011):
- Type 2 diabetes
- cardiovascular disease. Despite the fact that the population’s weight has increased, the frequency of cardiovascular disease has decreased. One of the reasons for this may be favourable trends in cholesterol and other fatty substances in the blood, decreases in blood pressure and fewer smokers (Sulo, 2013).
- certain types of cancer
- stop breathing at night (sleep apnoea)
- osteoarthritis of the hip and knee
- stigmatisation, mental disorders and unhappiness
However, the risk of osteoporosis and fracture is lower in people with obesity than in lean people (Søgaard, 2016).
Disease burden and deaths
High BMI is one of the top ten risk factors for death and contributed to four million deaths worldwide in 2015 and about 2400 deaths in Norway. The deaths in Norway were caused by cardiovascular disease (about 1500 deaths), cancer (about 500 deaths) and diabetes (approximately 400 deaths).
Among all BMI-related deaths from diabetes, most people had a BMI ≥ 30 kg / m2 (GBD 2015 Obesity Collaborators, 2017, GBD Compare, 2017).
In the age group over 65, we find the lowest mortality rate at a slightly higher BMI than among younger people (Kvamme, 2012).
Among adults, abdominal fat is more closely associated with type 2 diabetes and cardiovascular disease than general obesity (BMI over 30). Also in children, abdominal obesity is seen in conjunction with the increased risk of these diseases (Maffeis, 2008).
Factors that can increase the risk of overweight and obesity
Birth weight and weight increase among young children
High birth weight has the strongest correlation with the development of obesity in adulthood when parents have high BMI (Kristiansen, 2015; Glavin, 2014); it appears that there is only a small correlation between high birth weight and the development of obesity in adulthood (Evensen, 2017; Brisbois, 2012). This may therefore indicate that parental weight is more important for obesity development than the birth weight of the child.
From the age of two, obesity in childhood is clearly associated with increased risk of obesity in adulthood (Evensen, 2017; Glavin, 2014; Johannsson, 2006; Kvaavik, 2003; Magarey, 2003; Evensen, 2016; Whitaker, 1997). The risk increases with age and is even greater if one or both parents are obese.
Inactivity and high energy intake
At the population level, changes in the environment and lifestyle can explain the increase in the prevalence of overweight and obesity over the last decade. We live in a society that encourages physical inactivity, with a wide and tempting range of food. These are two factors that increase the risk of overweight and obesity, see the section about prevention below.
Association between mental disorders and obesity
Mental disorders can affect appetite, will and self-control, all of which are important factors for explaining the development of obesity. People who are affected by anxiety, depression and psychoses are also more vulnerable to experiencing stress and helplessness when facing challenges. This can lead to a further regulation of appetite and satiety and a higher intake of nutrient-poor foods that are rich in fat, sugar or salt.
Population studies among adults show that there is a higher proportion of mental disorders such as anxiety and depression among people with obesity than in the general population (de Wit, 2010). Follow-up studies have shown that anxiety and depression increase the risk of obesity development. However, obesity also increases the risk of anxiety and depression (Berkowitz, 2011).
Also among children (Korczak, 2013; Anzman-Frasca, 2012), psychological problems increase the probability of subsequent obesity. An explanation may be that children with psychological problems have a higher intake of sugary foods and beverages (Vollrath, 2012)
Medicinal side effects can also explain some of the correlation between obesity and mental disorders. Several medicines used for serious psychiatric disorders can affect brain mechanisms that control appetite and metabolism, which in turn can lead to major weight gain (Carlat, 2012; Ferno, 2011).
Prevention and challenges
In order to be able to alter overweight and obesity at society level, population-focused and individual-focused interventions are necessary. Interventions at community level can have a wider reach and be more effective than individual interventions, such as encouraging individuals to control their weight.
Children and adolescents are particularly vulnerable and affected by their surroundings; family, childcare, school and the local community.
Internationally, there is an increasing discussion about which public health interventions can and should be used to reduce the proportion of overweight and obesity in the population. Population-focused interventions discussed in Norway include facilitating physical activity in schools and the local community, and reducing access to nutrient-poor foods such as sweetened drinks. Important interventions may be financial means, media and awareness campaigns, marketing regulations, portion sizes, changing the composition of industrial produced foods and developing new products with healthier ingredients, as well as labelling food as healthy with the keyhole symbol used in the Nordic countries (NIPH, 2017d).
Norway already has a special tax on sugar, and the Minister of Health and Care Services has established a group of representatives from the food and business sector, where the goal is to implement measures to improve diet in the population (HOD, 2016).
Norway has committed to the WHO's goal of reducing the prevalence of non-communicable diseases in the period 2010-2015. Interventions will be based on common risk factors, including overweight and obesity. Norway will measure and report to the WHO about indicators related to the development of overweight and obesity among adolescents and adults.
- National NCD strategy 2013-2017 (pdf - in Norwegian)
- NCD Global Monitoring Framework (WHO)